Antibiotics are used to kill or inhibit the growth of microorganisms, which are considered a boon in medical science. However, due to their irrational use, microorganisms are becoming resistant to these drugs worldwide. Moreover, in Bangladesh, antibiotics are being misused, leading to diminished efficacy. According to research conducted by a government agency, 76 percent of patients in the country are being given antibiotics without any disease monitoring. Similarly, antiviral, antifungal, and antiparasitic drugs are also being administered at high rates without proper disease monitoring.
This issue was highlighted in a study titled ‘Situation Analysis of Antimicrobial Use Among Allopathic Practitioners in Bangladesh’ by the Health Economics Unit of the Ministry of Health and Family Welfare.
The study revealed that 52 percent of patients in the country are taking antibiotics. The Health Economics Unit collected a total of 10,500 medical records from across the country and analyzed them. However, over six and a half thousand documents were retained for final evaluation, bringing the issue of antimicrobial usage to light.
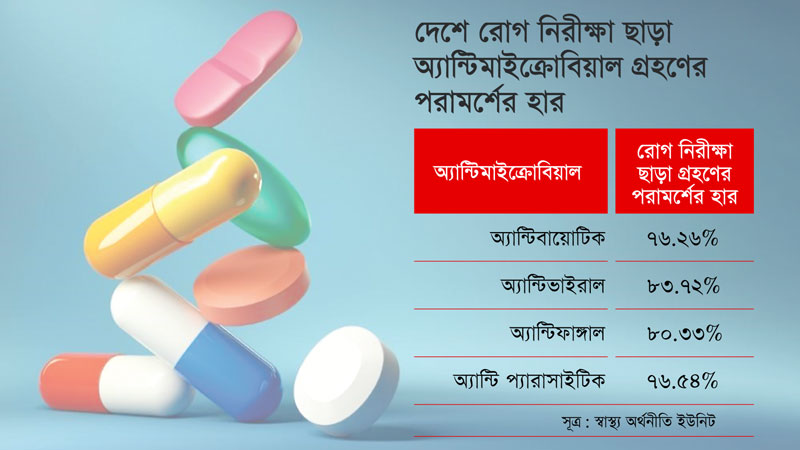
According to the study’s findings, 76 percent of patients were prescribed antibiotics without the physician examining the disease. The prescriptions analyzed in the study predominantly included antibiotics, with antivirals prescribed in 84 percent of cases, antifungals in 80 percent, and antiparasitics in 77 percent, all without disease screening.

Interestingly, prescriptions for antimicrobials were more prevalent among unqualified physicians compared to those with institutional degrees. Non-degreed physicians prescribed antimicrobials in 97 percent of cases without a diagnosis, while 83 percent of doctors with institutional degrees (at least an MBBS) prescribed antibiotics without a clinical examination. Furthermore, 73 percent of qualified doctors advised antibiotics without diagnosis, compared to 92 percent of unqualified doctors.
Experts emphasize that antibiotics are primarily intended for bacterial infections. However, at least a complete blood count (CBC) or whole blood test is necessary to confirm an infection. Doctors utilize CBC to gain a general understanding of whether an infection is present, assess blood cell levels, and determine hemoglobin levels. Additionally, blood culture is conducted to identify bacterial infections and determine the appropriate antibiotic. However, obtaining results from this test typically requires a minimum of 72 hours.
Many doctors prescribe antibiotics for conditions such as one-day diarrhea, where it’s challenging to ascertain whether the diarrhea results from an infection without testing. Although diarrhea often resolves within three days without intervention, antibiotics are frequently prescribed, even for colds and coughs.
Researchers observe that doctors often prescribe antibiotics without proper disease monitoring. While it’s not definitive that prescribing antibiotics without examining the disease is always incorrect, experienced doctors may make such decisions based on symptoms and disease duration, particularly if a patient has visited multiple times for treatment.
Dr. Subrata Pal, the focal person of the Bangladesh National Health Account Cell within the Health Economics Unit, highlighted that the study aimed to develop disease-specific cost information and analyze antimicrobial usage among mainstream allopathic physicians in the country. The study emphasized doctors with at least an MBBS degree as qualified, while those without such credentials were considered incompetent. However, the study did not previously explore the percentage of patients prescribed antibiotics without monitoring, indicating a need for further research to discern whether this pattern is commonplace or anomalous.
According to the Health Economics Unit’s study, antibiotic usage is highest among children, with unregistered doctors often advising patients to take antibiotics. In 83 percent of cases, patients received antibiotic prescriptions based on advice from unregistered doctors.
According to the World Health Organization (WHO), antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites change over time, becoming unresponsive to drugs, which makes infections difficult to treat. This escalation poses an increased risk of disease spread, serious illness, and death. The greatest threat to global health, food security, and development is bacterial antibiotic resistance. Antimicrobial resistance can affect people of any age in any country. Although resistance to antibiotics occurs naturally, humans have unnecessarily accelerated the use of antibiotics. This acceleration has led to increasing difficulties in treating infections such as pneumonia, tuberculosis, gonorrhea, and salmonellosis. AMR ranks among the top 10 public health threats worldwide.
Former Director-General of the Department of Health and medicine expert, Professor Dr. MA Faiz, commented that why antibiotics have been suggested cannot be determined solely by looking at the doctor’s prescription. He told Bonik Barta that doctors in our country usually do not mention the name of the disease, the diagnosis, and in many cases, the condition after the diagnosis on the prescription. In Bangladesh, there are a little more than 100,000 doctors registered with the Bangladesh Medical and Dental Council (BMDC). In addition to this number, several lakhs of people are treated as doctors. Many doctors are available in villages, slums, and remote areas. These issues should be considered in research. Antibiotics should not be administered if there is no infection in the patient’s body. To ascertain this, doctors should engage with the patient, assess symptoms, and conduct a thorough examination. Infections have various causes, and antibiotics should only be administered after some routine and specialized tests. Blood culture is particularly vital in this regard. At least two tests should be conducted before administering antimicrobials. However, such practices are not widespread in many cases in Bangladesh. If the doctor deems it necessary, antibiotics may be prescribed, but in such cases, one must be entirely certain about the infection. Moreover, there are protocols and guidelines for antibiotic usage, specifying which antibiotics should be administered for which disease. The Department of Drug Administration has also instructed against selling antibiotics to anyone without a doctor’s prescription. However, pharmacies in the country often disregard such instructions. The issue of antimicrobial resistance resulting from inappropriate antimicrobial use is not insignificant.
Former president of the Bangladesh Medical Association (BMA) and president of the National Committee of the Health Rights Movement, Prof. Dr. Rashid-e Mahbub, told Bonik Barta that microbial infection can be diagnosed through blood culture. He believes doctors consider this aspect. Patients often visit doctors with symptoms like fever and bleeding, expecting antibiotics for treatment. Doctors prescribe antibiotics to address these expectations. Simultaneously, patients are reluctant to revisit doctors who do not prescribe antibiotics. The mentality of those seeking treatment also plays a role. This scenario differs in developed countries where they have robust management systems. Antibiotics are not readily available, and doctors there may ask patients to wait at least 48 hours before prescribing antibiotics. However, adopting such practices in Bangladesh might result in the loss of patients for doctors. The health sector in Bangladesh faces challenges, and public hospitals typically prescribe fewer antibiotics due to limited antibiotic supplies. Antibiotics are not sold without a doctor’s prescription, and doctors are cautioned against prescribing antibiotics without evidence. Prof. Dr. Rashid-e Mahbub emphasizes the importance of sound health management, stressing that there is no substitute for it.