In three decades, the number of hospitals and diagnosis centers under government and private management in the country has increased at a significant rate. However, at this time, radiation and waste management were not properly developed in health care institutions. Consequently, people living in the vicinity of health care facilities for a long time are at risk of health problems. Cancer, heart disease, damage to reproductive health, and the spread of infectious diseases are creating various risks. Public health experts say that these issues remain out of control.

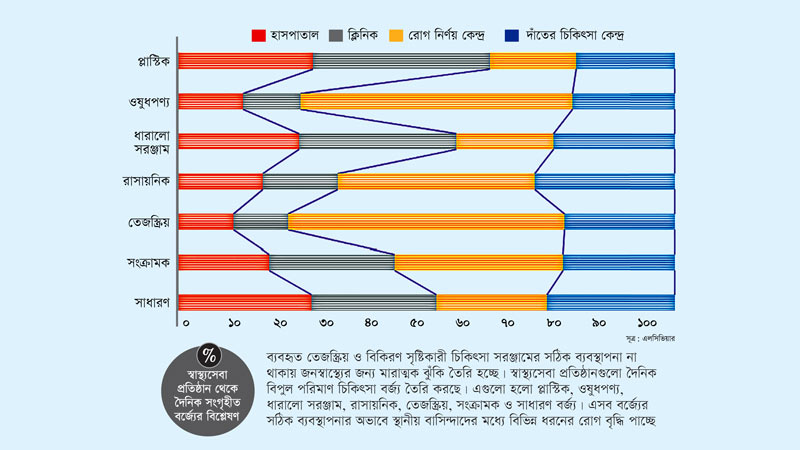
They assert that the use of radiation in diagnosis is a major discovery in medicine. However, due to the lack of proper management of the used radioactive and radiation-generating medical equipment, there is a serious risk to public health. Healthcare institutions generate huge amounts of medical waste daily, including plastics, drugs, sharp tools, chemicals, radioactive, infectious, and general waste. Due to the inadequate management of these wastes, various diseases are increasing among local residents. Some diseases develop quickly, while others manifest after a long time.
According to the World Health Organization (WHO), more than 15 percent of the total waste generated in healthcare activities is infectious, toxic, or radioactive. Although 1.6 billion injections are administered worldwide each year, not all needles and syringes are properly disposed of. Incineration of some medical wastes also releases dioxins and particulate matter. The organization believes that if safe management of these wastes is not ensured, health and environmental risks may increase.
A recent study found that exposure to radiation in the nation’s hospitals is increasing the lifetime risk of cancer among local residents and those treated and diagnosed with the disease. Radiation affects living cells in the human body, damaging genetic material (DNA) and reproductive cells. The US-based scientific journal Hillion published the research paper in September this year. In the study entitled ‘Assessment of Radiation Level and Potential Risk to Public Living Around Major Hospitals in Central and Western Bangladesh,’ radiation data from 10 public and private hospitals were collected. These include Bangabandhu Sheikh Mujib Medical University, Dhaka Medical College Hospital, National Cancer Research Institute Hospital, Shaheed Suhrawardy Medical College Hospital, Sir Salimullah Medical College Mitford Hospital, Rajshahi Medical College Hospital, Khulna Medical College Hospital, and the top three private hospitals of the capital.
According to the study, the International Commission on Radiological Protection (ICRP) recommended a tolerable level of risk of 0.57 microsieverts (measurement of radiation and radioactivity), and the recommended tolerable level of risk for Biological Effects on Ionizing Radiation (BEIR) is 0.64 microsieverts. However, the amount of radiation generated from hospitals in the country is several times higher. Radiation dose rates in the hospitals during the study ranged from 0.012 to 0.355 microsieverts. The annual dose ranges from 0.21 millisieverts to 622 millisieverts. However, the radiation dose rate of the 10 hospitals mentioned in Bangladesh during the study was higher than that of Nigeria, India, and Switzerland.
The study pointed out that these health risks are mainly due to a lack of knowledge of radiation protection and radiation protection of healthcare workers, lack of modern radiation production equipment, and excessive stress on the patient. Additionally, issues of inadequacy in quality control of radiation-producing equipment in the absence of qualified physicists in private diagnostic centers near big hospitals have also been highlighted in the study.
Radiation experts say that ionizing radiation is used in medicine, industry, and agricultural research in Bangladesh. Radiation workers and the public are at risk from ionizing radiation used for treatment. Although hospital radiation workers are routinely monitored for radiation with thermoluminescent dosimeters (TLDs), there are no comprehensive studies to estimate the radiological risk of locals living in hospital areas. Among the diagnostic procedures, X-rays and CT scans carry the highest risk. The private clinics and diagnostic centers that have emerged in the poor and rural areas of the country also lack proper management.
President of Bangladesh Cancer Society Professor Dr. Golam Mohiuddin Farooq told Bonik Barta, “There is a shortage of radiotechnologists in the country. The shortage of technologists in radiotherapy, X-ray, and CT scan is being filled to some extent. Lack of skilled manpower and existing manpower is retiring, but new manpower is not being created. Most of the hospitals, clinics, and diagnostic centers have poor infrastructure. As a result, there is no preparation for radiation control. Regular inspections by the Atomic Energy Regulatory Authority are supposed to ensure the safety of doctors and technologists working with radiation. However, there is a lack of discussion on addressing radiation issues.
CT scans produce 34 percent of the total radiation dose, according to research data. Although ionizing radiation has no immediate effect on human health, it increases the risk of cancer later. Gamma radiation is the most dangerous of the radiations, capable of completely passing through the human body, and can cause long-term health risks such as cancer, DNA damage, cardiovascular disease, and gene mutation.
Harvard Medical School in the US raises questions about the intensity of radiation from medical imaging. Many experts are concerned about the use of high radiation dose tests, such as X-rays, CT scans, and nuclear imaging. While CT scanning and nuclear imaging have revolutionized diagnosis and treatment, many are invasive and pose potential risks. The radiation in X-rays, CT scans, and nuclear imaging is ionizing radiation (high-energy wavelengths or particles that penetrate tissue and expose the body’s internal organs and structures), which can damage DNA, potentially leading to cancer.
Hundreds of tonnes of medical waste are generated daily from public and private healthcare institutions in the country, most of which pose serious health and environmental risks. Needles, syringes, and bandages pose potential infection, disease, and health hazards. Moreover, these wastes contribute to environmental pollution.
A Netherlands-based scientific journal, Elsevier, published a research paper this year stating that an average of one to two and a half kilograms of waste is generated per hospital bed across the country. The study titled ‘Healthcare Waste in Bangladesh: Current Status, the Impact of Covid-19 and Sustainable Management with Life Cycle and Circular Economy Framework’ reveals that more medical waste is generated in Dhaka than in any other region of the country. At least 50 tons of medical waste are generated in this city per day, with 26 percent of it being classified as dangerous. These wastes vary in quantity across different seasons. Generally, residential hospitals generate more waste than pathological labs and diagnostic centers, with diagnostic centers primarily generating chemical, infectious, and radioactive waste.
Public health expert Dr. Lelin Chowdhury emphasized, “A large number of people have a vague idea about the radiation that emanates from the X-ray room. The Atomic Energy Commission determines the specifications, such as the thickness of the full wall the door should have, whether it should be wrapped with lead or lath, and how thick it should be. There is special clothing for the person conducting the X-ray or CT scan. Conducting radiation activities without adhering to the commission’s standards and certifications is punishable by law.”
Regarding waste management, Dr. Chowdhury added, “Medical waste management has been developed in major cities including Dhaka. Institutions generating medical waste use different colored bins. These wastes are managed under a tripartite agreement between the City Corporation or Prism Bangladesh, and the hospital where the waste is generated. Those who do not adhere to this management system can pose risks and should face punitive action.”
Director-General of the Department of Health, Abul Bashar Mohammad Khurshid Alam, commented that the government is aware of medical waste management. He told Banik Barta, “Medical waste management is a recognized issue worldwide. Improper management poses a threat to public health. Government guidelines for proper medical waste management exist, and local governments and private organizations are working towards this goal. While proper waste management may be observed at hospitals, disposal practices may not align with intentions. The government is undertaking waste management projects alongside addressing other issues. The government is cognizant of medical waste management, and while the risk of damage due to radiation is low, those working with radiation are taking protective measures. However, more research is needed on the potential impact on individuals living near hospitals.